DNR by another name
Today's Caregiver Tip Tuesday blog comes from the New York Times " New Old Age" Blog and was written by Paula Span.
"I'd like to bring you up to speed on what's going on," the doctor said. He had a red goatee and was wearing a white coat. He said that my father had pneumonia and needed a "breathing machine," and that he also had sepsis and acute lung injury. "The statistics are not too good," he said solemnly. "Around 40 percent of people who are just like him will die from this."
I felt anxious even though this "doctor" was actually an actor in a video simulation devised by University of Pittsburgh researchers to see how physician communication affects end-of-life decisions. The situation he described is common in I.C.U.'s and not so different from what I confronted when my father actually went to an emergency room last winter.
The "doctor" eventually asked whether, as my relative's surrogate, I wanted the staff to perform CPR if his heart stopped. He pointed out that only about 10 percent of such patients receiving CPR would survive.
"It's a very vulnerable time," said Amber Barnato, the preventive medicine specialist who helped develop the experiment. "A turn of phrase by a doctor can make a lot of difference."
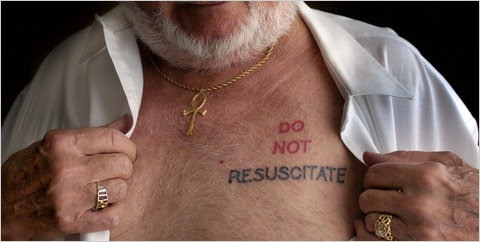
Dr. Barnato's study, just published in the journal Critical Care Medicine, drew my interest because of one of those phrases: "allow a natural death." Both she and I had read the same article in a nursing journal a few years ago, proposing to substitute this wording for "do not resuscitate."
The author, a nursing educator, had found that medical professionals liked the new wording. But what about family members faced with the decision? Would they be more likely to consent to or decline CPR depending on whether the medical order was "do not resuscitate" versus "allow natural death"? Dr. Barnato proposed to find out.
(Brief digression: It's interesting how often a particular patient, vividly remembered, sparks a researcher's efforts. When she was an intern, Dr. Barnato told me, a woman in her 80s, suffering from a serious stroke and sepsis, communicated — by writing and blinking — that she wanted to be removed from a ventilator. Instead, the woman got a psychiatric evaluation, Prozac and, eventually, bilateral chest tubes, a feeding tube and a tracheostomy before being moved to a long-term care facility. Interns don't have much authority in such cases, but Dr. Barnato, feeling "morally distressed," embarked on 15 years of research into end-of-life practices.)
The video simulation I saw was viewed by 252 people, a nonrandom sample of volunteers from eight cities (average age: 50) who actually were designated health care surrogates for parents or spouses. In this hypothetical case, they listened to the "doctor" say various things, then decided: CPR? Or DNR?
Most agreed to CPR, despite low odds of survival: 56 percent was the average. Some manipulations had little effect on that decision. Being emotionally aroused — by a photo of a loved one and an exercise designed to prompt memories of him or her — didn't make participants more or less likely to choose CPR.
Nor did sympathetic expressions from the "doctor." In some simulations, he said things like, "This must feel really overwhelming to have everything happen so suddenly." It didn't significantly change decisions.
Nor, to Dr. Barnato's surprise, did framing the decision as what the patient would want, as opposed to what the surrogate wanted.
So what did make a difference? Two factors:
• What other people reportedly chose. When the guy in the white coat says that in his experience, most people want CPR, 64 percent of surrogates said yes to it. When he says that most people don't want it, the proportion dropped to 48 percent.
"A person who is acting with very little knowledge might think, 'Those other people know something,'" Dr. Barnato theorized. "The standard choice is what people will choose. That's what's 'normal.'"
• The phrase "allow a natural death." Even though they mean the same thing in this experiment, when the fake doctor framed the option as "do not resuscitate," 61 percent asked that CPR be performed. But only 49 percent of participants wanted CPR when asked if the staff should "allow a natural death."
"It sounds kinder and gentler," Dr. Barnato said. By contrast, DNR suggests withholding or relinquishing, "the feeling of not getting something." Besides, "we like 'natural' things," she added.
As many commenters pointed out the last time we discussed this, the phrase may be too vague for physicians' comfort. They want specifics, and a document like those known as "physician orders for life-sustaining treatment" provides specifics more effectively than "allow a natural death."
But family members? Based on this first, small experiment, they like the sound of it.